Non-Small Cell Lung Cancer (NSCLC) is a very common type of cancer, and despite currently available therapies, is one of the deadliest due to the emergence of drug resistance, which results in tumor recurrence. Thus, there is a clear need for novel therapeutic strategies to overcome resistance, especially in the EGFR+ cohort of patients. The group of Prof. Yosef Yarden has developed a new therapeutic antibody that blocks a common drug resistance mechanism. This antibody completely inhibited tumor progression and was proven especially efficient when administered in combination with known drugs by inhibiting drug resistance thus preventing relapses of NSCLC.
Lung cancer is one of the most deadly and common types of cancer in the world. Non-Small Cell Lung Cancer (NSCLC) accounts for about 85% of all lung cancers. Several lines of therapies exist, including targeted therapies that inhibit specific signaling pathways such as EGFR inhibitors. However, although targeted therapy in NSCLC has provided disease control, the tumors inevitably develop drug resistance, leading to tumor recurrence and disease progression.1 The low cure rate and serious side effects call for novel therapeutic strategies and combinatorial treatments against lung cancer.
The group of prof. Yosef Yarden has developed a new antibody that inhibits a receptor that is known to induce drug resistance.
Overexpression of Anexelekto (AXL), a Receptor Tyrosine Kinase (RTK), is associated with poor prognosis and it is known to induce resistance to chemotherapies and targeted therapies. The group of Prof. Yosef Yarden has developed a new anti-AXL antibody (mAb654) that recognizes human AXL, blocks it from binding its ligand (GAS6), downregulates receptor expression and inhibits both receptor activation and downstream signaling. Most importantly, mAb654 limited tumor growth in-vitro and in-vivo. Using a widely accepted animal model of NSCLC that evolves resistance to kinase inhibitors, they showed that a combination of EGFR-specific Tyrosine-kinase inhibitor (osimertinib) and cetuximab (anti-EGFR) with mAb654, completely inhibited tumor progression and prevented relapses in animal models (Figure 1), including patient-derived xenografts. Therefore, mAb654 fully inhibits the emergence of resistance to EGFR kinase inhibitors.
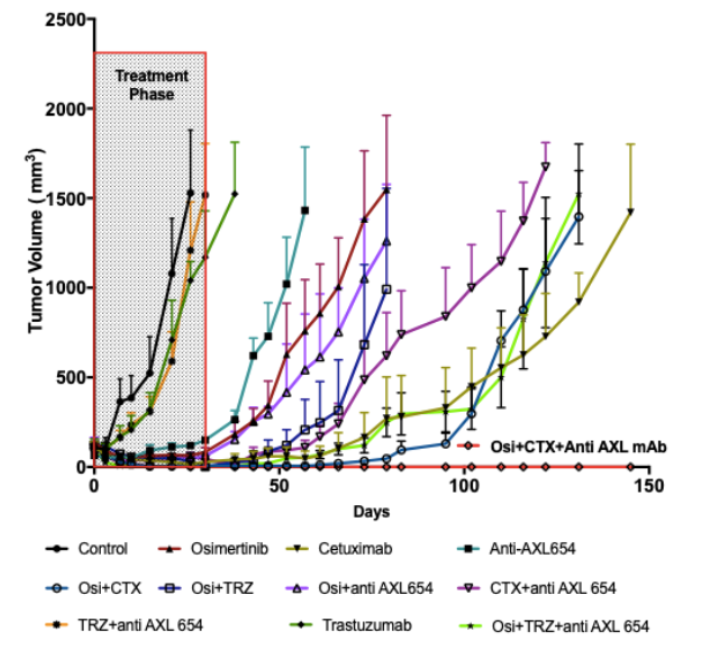
Figure 1 - In an animal model, simultaneous interception of EGFR and AXL is essential for complete cure of drug-resistant NSCLC cells. PC9 human NSCLC cells were engrafted in CD-1 nu/nu mice. When the tumors became palpable, mice were treated with the indicated drugs, either daily (osimertinib; 5mg/kg) or once every three days (anti-AXL mAb654, cetuximab or trastuzumab; 200ug/mouse/injection). Data are ± SEM from 10 mice in each group.
- A new effective treatment for NSCLC
- Prevents relapses of NSCLC
The team developed the antibody, characterized its mechanism of action in vitro and in vivo, and developed a new method for combination therapy which was tested in a mouse model.
References:
Yuan M, Huang L-L, Chen J-H, Wu J, Xu Q. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct Target Ther. 2019;4(1):6 doi:10.1038/s41392-019-0099-9


